Antibiotics are drugs that kill or inhibit the growth of bacteria and are indispensable in the fight against bacterial infections.
Although they have saved millions of lives from diseases such as pneumonia and sepsis, their inappropriate use poses a serious risk to both individual health and society. Today, the harm of antibiotics is becoming an increasingly urgent problem, as their excessive or inappropriate use leads to increased bacterial resistance, the loss of beneficial intestinal bacteria and the development of various complications. In this article, we will discuss the main threats posed by antibiotics and provide practical advice on how to protect yourself and contribute to the preservation of public health by strengthening natural immunity and using appropriate nutritional supplements.
Understanding the causes of antibiotic harm
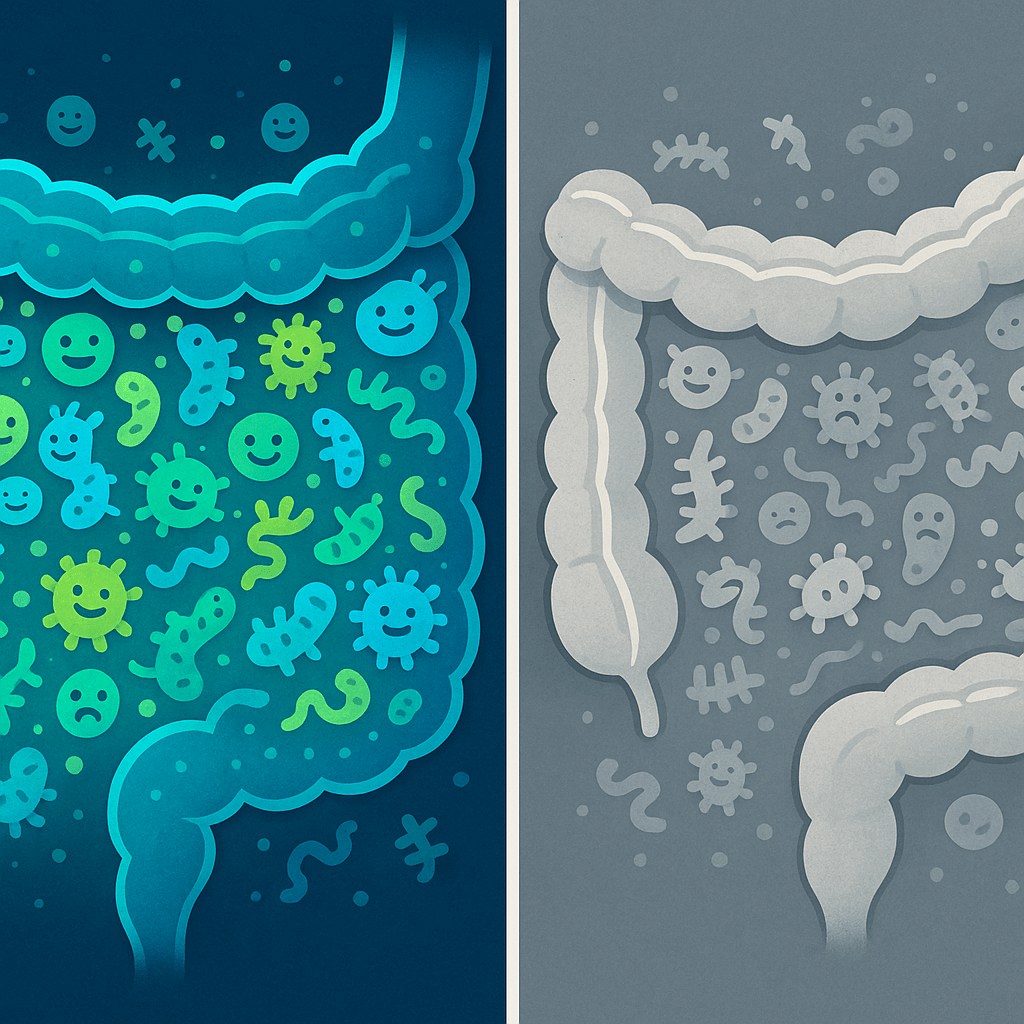
Antibiotics work purposefully – they kill or inhibit the growth of bacteria that have caused an infection. However, the problem is that these drugs often cannot distinguish between “bad” bacteria and “good” bacteria that are vital to our body. When we take antibiotics, they affect all bacteria – both pathogenic microorganisms and beneficial bacteria that make up our intestinal microflora.
One of the biggest problems is the inappropriate use of antibiotics to treat diseases caused by viruses. The World Health Organization (WHO) emphasizes that antibiotics are completely ineffective in fighting viruses, such as colds or flu. Despite this, many people try to treat themselves with antibiotics at the first symptoms of a cold.
As the infectious disease doctors of Vilnius University Hospital Santara Clinics explain, the effect of antibiotics on the body is twofold: they not only fight the infection, but also cause changes in the entire body system. That is why it is very important to use them only when absolutely necessary and strictly according to the doctor’s instructions.
Bacterial and viral infections: what is the difference?
In order to understand the proper use of antibiotics, it is important to clearly distinguish between bacterial and viral infections:
- bacterial infections are caused by bacteria – single-celled microorganisms that can reproduce independently and are sensitive to antibiotics;
- viral infections are caused by viruses – even smaller pathogens that cannot reproduce independently and are not sensitive to antibiotics.
According to the Ministry of Health of the Republic of Lithuania, as many as 70% of upper respiratory tract infections are caused by viruses, therefore prescribing antibiotics in these cases has no positive effect, but only increases the damage to the body and promotes the development of resistant bacteria.
Common antibiotic risks and side effects
Antibiotic side effects can range from mild digestive upset to severe, life-threatening conditions. According to the European Centre for Disease Prevention and Control, about 20% of patients taking antibiotics experience at least one adverse reaction.
- Antibiotic resistance is one of the most serious public health threats. Bacteria adapt and become resistant to drugs, making infections more difficult to treat.
- Damage to the intestinal microflora – antibiotics destroy not only pathogenic but also good bacteria, which causes digestive disorders, constipation, diarrhea or even the development of pseudomembranous colitis.
- Allergic reactions – from mild skin rash to anaphylactic shock, which can be fatal.
- Organ damage – some antibiotics can cause liver, kidney or even hearing damage, especially when used in high doses or for a long time.
- Vitamin deficiency – especially B vitamins, as antibiotics disrupt their absorption and production in the intestine.
- Weakening of immunity – due to impaired intestinal microflora, which plays an important role in the immune system.
As noted by gastroenterologists of the Lithuanian University of Health Sciences Hospital Kaunas Clinics, after a course of antibiotics, the intestinal microflora may take from several weeks to several months, and in some cases even years to recover. During this period, the body becomes more vulnerable to various infections.
How to avoid the dangers of antibiotics?
Responsible use of antibiotics is the main way to avoid the harm they cause.
It is important to understand that antibiotics are prescription drugs, the use of which should be strictly controlled by healthcare professionals.
Here are the main recommendations that will help reduce the harm caused by antibiotics:
- Take antibiotics only when prescribed by a doctor. Never self-medicate with antibiotics or take them from friends/family members.
- Always complete the entire prescribed course. Even if you feel better, stopping treatment early allows resistant bacteria to survive and multiply.
- Follow the dosage exactly. Take the medication exactly as prescribed – no more, no less.
- Combine with probiotics. After consulting with your doctor or pharmacist, take probiotics during or after a course of antibiotics to restore the intestinal microflora.
- Eat well and drink enough fluids. This will help the body recover faster after a course of antibiotics.
- Strengthen your immunity naturally. Exercise regularly, get enough sleep, avoid stress, and ensure sufficient vitamin levels in the body.
The recommendations of the Lithuanian Society of Infectious Diseases emphasize that it is important not only to use antibiotics correctly, but also to pay attention to the restoration of the body after their use. The digestive system is particularly vulnerable, therefore it is recommended to ensure effective care of the digestive system by using special food supplement formulas.
Food supplements and natural remedies after antibiotics
To restore the body after a course of antibiotics, it is recommended:
Probiotics and prebiotics. Probiotics are live bacteria that help restore the intestinal microflora. Prebiotics are dietary fibers that feed the good bacteria. The best time to take probiotics is 2-3 hours after a dose of antibiotics, or as prescribed by a doctor.
- Vitamins and minerals:
- Vitamin C – strengthens immunity and helps restore the intestinal mucosa
- Vitamin D – essential for the immune system
- B vitamins – often depleted after a course of antibiotics
- Zinc – important for the normal functioning of the immune systemVit
- Fermented products:
- Kefir and yogurt with live cultures
- Sauerkraut and other vegetables
- Kombucha – fermented tea
- Kimchi – a dish of fermented vegetables
- Fiber: whole grains, vegetables, fruits, seeds – they feed the beneficial bacteria in the gut.
For effective immunity boosting after a course of antibiotics, especially for children and adults who find it difficult to take traditional pills, it is recommended to choose vitamin gummies to boost immunity, which are a pleasant and effective alternative.
How to recognize when antibiotics are not needed?
Patients often demand antibiotics even when they are not needed – especially in the case of a cold or flu. It is important to be able to recognize situations when antibiotics are not an appropriate treatment.
Here are the main signs that you probably have a viral illness that does not require antibiotics:
- Runny nose, cough, and sneezing without fever or with a low fever
- Sore throat without white plaque on the tonsils
- Painful sinuses with clear discharge
- Symptoms that last less than 10-14 days
- Fever that goes away within 2-3 days
Signs of a bacterial infection that may require antibiotics:
- High temperature (over 38°C) that lasts longer than 3 days
- Green or yellow, thick nasal discharge that lasts longer than 10-14 days
- Severe sore throat with white plaque on the tonsils
- Severe earache or discharge from the ears
- Symptoms that improve and then significantly worsen
The recommendations of the Lithuanian College of Family Physicians emphasize that it is always worth consulting a doctor before starting antibiotics. In the case of a cold or flu, it is better to focus on relieving symptoms and strengthening immunity with natural supplements and vitamins than to take antibiotics, which will not help, but only harm the body.
The irrational use of antibiotics is one of the biggest public health problems, contributing to the development of resistant strains of bacteria. The European Centre for Disease Prevention and Control predicts that by 2050. more people in Europe could die each year from infections caused by antibiotic-resistant bacteria than from cancer, if the situation does not improve.
Conclusions
The use of antibiotics, while necessary in certain cases, should always be well thought out and monitored by medical professionals. The harm that can be caused by inappropriate or excessive use of antibiotics often outweighs the benefits, especially when they are prescribed for the wrong diagnosis.
- It is important to remember a few basic principles:
- Take antibiotics only when prescribed by a doctor
- Always complete the prescribed course of treatment
- Protect and restore your intestinal microflora
- Strengthen your immunity with natural means
- Contribute to the fight against antibiotic resistance by using them responsibly
Our health and the effectiveness of medicine for future generations depend on the decisions we make today. By taking care of our immunity, taking medications properly, and prioritizing prevention, we can avoid many of the problems associated with antibiotics and ensure that these important medicines remain effective in the future.
Frequently Asked Questions
What are the main side effects of antibiotics?
Antibiotics can cause an imbalance in the intestinal microflora, allergic reactions, digestive disorders, vitamin deficiencies and contribute to the development of resistant bacteria if used incorrectly.
How to restore gut health after antibiotics?
Include probiotic-rich foods in your diet, eat plenty of fiber, drink enough water and consider taking approved probiotic supplements to help your recovery.
Can antibiotics treat viral infections?
No, antibiotics are only effective against bacterial infections, they have no effect on viruses that cause colds or flu.
What should you do if you suspect a side effect of antibiotics?
Contact your doctor immediately – never adjust the dose or stop treatment yourself.
How can you prevent antibiotic resistance?
Only take antibiotics when prescribed by a doctor, always complete the full course of treatment, and never share antibiotics or take them on your own.