Arthritis is a common condition that can affect people at various stages of their lives. It is not just a temporary discomfort, but a serious problem that can significantly reduce the quality of life. Each person’s experience with arthritis can vary, from short-term pain to chronic, long-term symptoms that limit movement and daily activities.
Interestingly, temporary joint pain does not necessarily mean that there is an inflammatory process – it can simply be the result of muscle strain or fatigue. However, when you experience persistent pain, swelling, or other signs of inflammation in your joints, it is important to consult a specialist to find out the real cause. If you are interested in natural ways to strengthen your joints, learn about vitamins for joints and how supplements such as collagen and vitamin D can be beneficial.
In this article, you will learn about the causes of arthritis, the main symptoms, diagnostic methods, and various treatment options – from traditional medicines to natural remedies that help relieve pain and improve your quality of life.
What is arthritis?
Joint inflammation, medically known as arthritis, is a condition in which the body’s immune system becomes inflamed in the joints. It is not a single disease, but rather a condition that encompasses a number of different disorders that all cause joint pain and impair function.
The main types of joint inflammation are:
- Osteoarthritis is the most common type of joint disease, characterized by the breakdown of cartilage in the joints, most commonly affecting the knees, hips, hands, and spine.
- Rheumatoid arthritis is an autoimmune disease in which the body’s immune system mistakenly attacks joint tissue, causing chronic inflammation and deformity.
- Gout is a metabolic disorder in which uric acid crystals build up in the joints, causing acute, intense pain, most commonly in the big toe joint.
- Bursitis is inflammation of the bursa, a sac that cushions the joints and reduces friction between bones, tendons, and muscles.
- Ankylosing spondylitis is a chronic inflammatory disease that primarily affects the spine and sacroiliac joints.
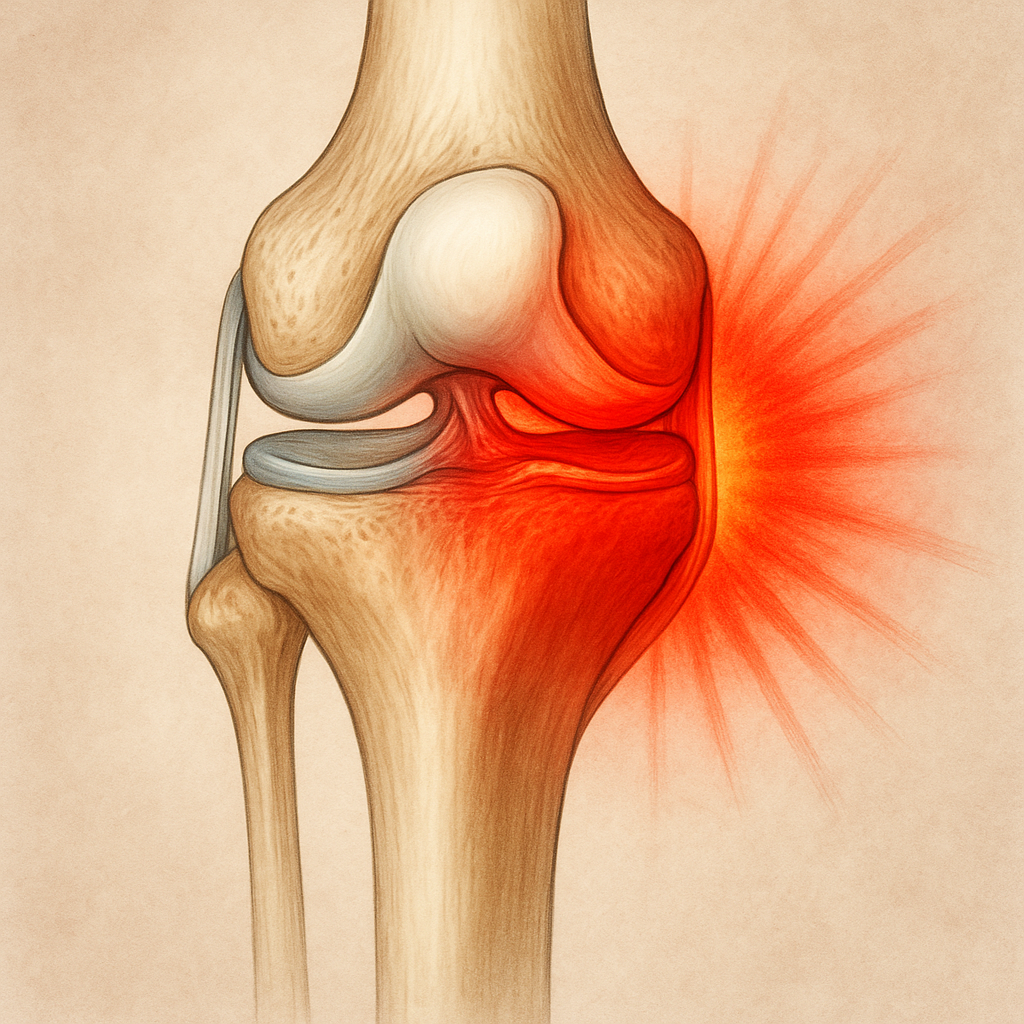
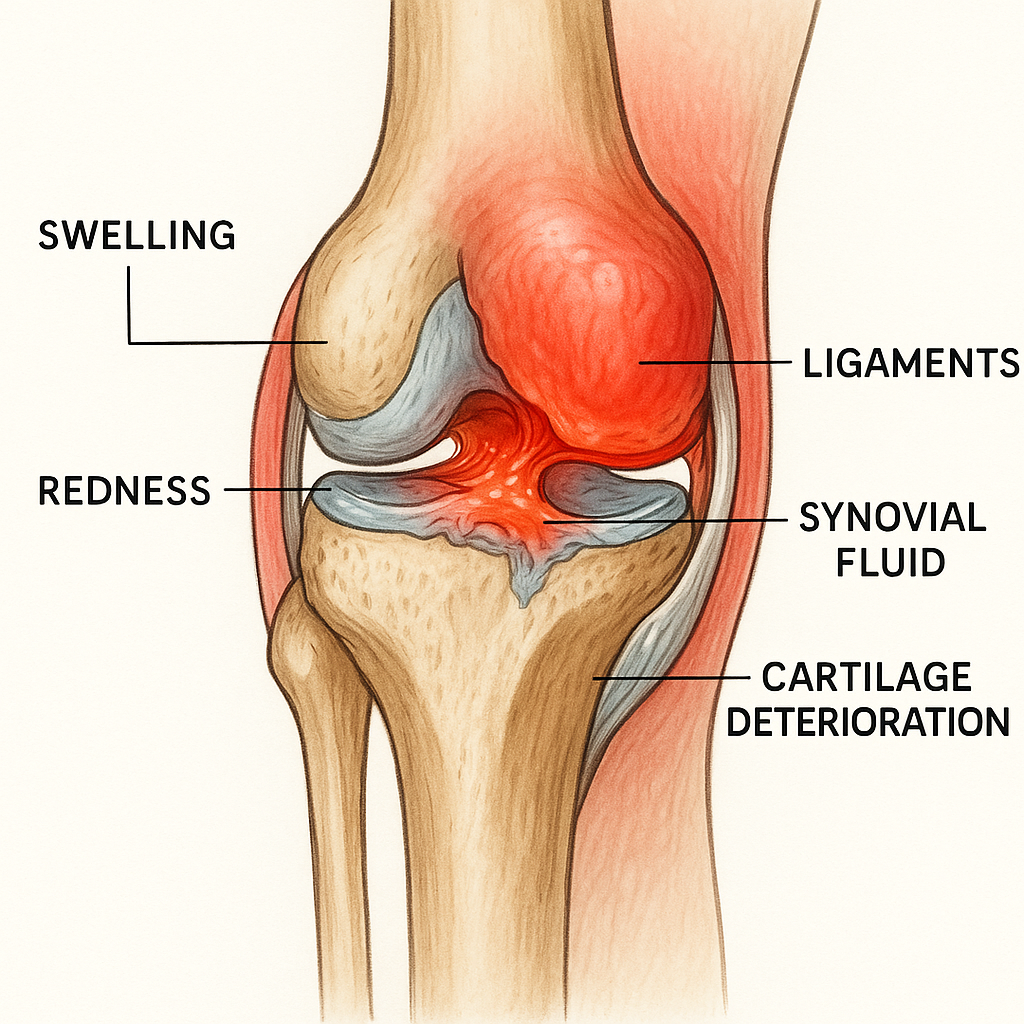
In human joints, there is synovial fluid between the bones, which acts as a lubricant, reducing friction during movement. In cases of joint inflammation, the production of synovial fluid is disrupted, swelling occurs, and cartilage – the soft, elastic tissue that covers the ends of bones – begins to break down. This process causes pain, stiffness, and can eventually limit the mobility of the joint.
Joint inflammation can be acute (short-term) or chronic (long-term). Acute inflammation is often caused by an injury or infection and usually resolves with treatment of the underlying cause. Chronic inflammation, on the other hand, can last for months or years, requiring long-term treatment and care. For more information on related movement and joint conditions, see our explanation of the causes of joint pain for patients and caregivers.
Causes of joint inflammation
Joint inflammation can be caused by a variety of factors, depending on the specific disease or condition. Understanding the underlying causes can help you better manage the condition and choose the most appropriate treatment.
Degenerative causes
Osteoarthritis, the most common form of arthritis, usually develops as a result of the natural aging process and the wear and tear of joint cartilage over time. Over time, the cartilage that covers the ends of bones in joints thins and wears away, causing the bones to rub against each other, causing pain, inflammation, and movement problems.
Autoimmune causes
Rheumatoid arthritis and other inflammatory forms of arthritis occur when the body’s immune system inappropriately attacks joint tissue. In this case, white blood cells that are supposed to fight infection accumulate in the joints, causing inflammation, pain, and eventually structural damage.
Metabolic factors
Gout is a metabolic disorder characterized by too much uric acid in the blood (hyperuricemia). When the body cannot properly remove uric acid, its crystals build up in the joints, most often at the base of the big toe, causing intense pain and inflammation.
Infectious causes
Septic arthritis develops when bacteria, viruses, or fungi enter a joint, causing infection and inflammation. This condition usually affects one joint and requires urgent medical attention because it can cause long-term joint damage.
Injuries and Overuse
Joint injuries, such as dislocations, sprains, or fractures, can cause acute joint inflammation. Repetitive motion or prolonged stress on the joints, especially during work or sports, can also lead to chronic inflammation.
Lifestyle factors
Obesity is a significant risk factor for developing osteoarthritis, especially in weight-bearing joints such as the knees and hips. Certain foods can also promote inflammation in some people, especially those with gout. Lack of physical activity can also contribute to joint problems by weakening the muscles that support the joints.
Seasonal and environmental factors
Many people with arthritic conditions find that their symptoms worsen in cold, damp weather or when the weather changes suddenly. Many people experience a worsening of their symptoms in the spring, when atmospheric pressure often fluctuates. Although the exact cause of this phenomenon is not fully understood, it is thought to be related to changes in the pressure of the joint fluid.
Genetic factors
Some forms of arthritis have a clear genetic component. For example, the risk of rheumatoid arthritis increases if there is a family history of the disease. In addition, certain genes related to the immune system may increase the risk of autoimmune forms of arthritis.
Supplements for pain and inflammation can complement your health care plan. Discover the best options in our catalog of pain and inflammation products.
Main symptoms and how to recognize them
Symptoms of joint inflammation can manifest themselves in different ways, depending on the type of inflammation, its intensity and the joints affected. Recognizing these symptoms is important because early diagnosis allows for faster initiation of appropriate treatment and reduces the risk of long-term damage.
Pain
- Pain is one of the main symptoms of joint inflammation. Its nature can vary greatly:
- Acute or dull – depending on the cause and stage of the inflammation
- Constant or episodic – some people feel constant pain, others only at certain times, for example in the morning
- Localized or diffuse – the pain may be felt only in the affected joint or spread to surrounding tissues
Swelling and visible inflammation
The affected joint is often swollen due to fluid accumulation at the site of inflammation. The swelling may be slight, noticeable only when compared to the unaffected joint, or severe, clearly visible and changing the shape of the joint.
Redness and warmth
A joint affected by inflammation may become warmer than the surrounding tissues due to increased blood flow to the area of inflammation. The skin over the joint also often turns red, which is the body’s natural response to inflammation.
Morning stiffness and limited range of motion
Many people with arthritis experience stiffness in their joints, especially after periods of rest, such as when they first get up in the morning. This stiffness can last from a few minutes to a few hours. Over time, the inflammation can limit the range of motion of the joint, making it difficult to fully bend or straighten the affected joint.
Systemic effects
Chronic inflammatory joint diseases can also cause systemic symptoms:
- Fatigue – a common symptom, especially in rheumatoid arthritis
- Fever – in some cases, especially in infectious arthritis
- Weight loss – chronic inflammation can affect appetite and metabolism
- General malaise – the body fights inflammation, so there is less energy left
| Type of arthritis | Typical symptoms |
| Osteoarthritis |
Pain that worsens with exercise and improves with rest
– Short-term morning stiffness (usually < 30 min.)
– Joint “cracking” during movement
– Joints most commonly affected: knees, hips, hands, back
– Prolonged morning stiffness (> 1 h.)
|
| Rheumatoid arthritis |
– Symmetrical joint damage (both hands, both feet)
– Damage to small joints (fingers)
– Systemic symptoms: fatigue, weakness, fever
– Rheumatic nodules under the skin
– Sudden, intense attacks of pain
– The base of the big toe is most often affected
|
| Gout |
– Severe redness, swelling, and warmth in the affected joint
– Attacks often begin at night
– Skin over the joint may peel
– Localized swelling and pain
|
| Bursitis |
– Most often affects the elbow, knee, shoulder, or hip
– Pain worsens with pressure or movement of the joint
– Redness is sometimes visible
|
For example, rheumatoid arthritis symptoms often involve both joints and non-articular symptoms – learn about these subtleties in our rheumatoid arthritis overview.
Diagnosing arthritis
Accurate and timely diagnosis of arthritis is essential for effective treatment. The diagnostic process is often complex and involves several different parts of the medical examination.
Patient history and symptom review
The first step in diagnosing arthritis is a thorough analysis of the patient’s history. Your doctor will ask questions about:
- The nature, intensity, and duration of your symptoms
- When your symptoms get worse or better
- Is there a family history of arthritis
- Your general health and comorbidities
- Current medication use
- Your lifestyle, including physical activity, diet, and unhealthy habits
Physical examination
Your doctor will perform a thorough physical examination, which will include:
- Examining the affected joints for swelling, redness, or deformity
- Assessing joint mobility and function
- Checking for pain on palpation or movement
- Looking for systemic signs of inflammation (such as fever)
Laboratory tests
Blood tests can reveal various inflammatory markers and help determine the specific type of arthritis:
- C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) – elevated levels indicate inflammation in the body
- Rheumatoid factor (RF) and anticyclic citrullinated peptide (ACCP) antibodies (anti-CCP) – helps diagnose rheumatoid arthritis
- Uric acid levels – elevated levels may indicate gout
- Antinuclear antibodies (ANA) – linked to autoimmune diseases
- Complete blood test (CBC) – can reveal infection or other abnormalities
In some cases, a joint puncture procedure (arthrocentesis) may be performed, in which fluid is removed from the joint for analysis. This is especially useful in diagnosing infectious arthritis and gout.
Imaging tests
Imaging tests help assess the structure of the joints and the extent of inflammation:
- X-rays – show bony structures and can reveal joint space narrowing, erosions or bony growths (osteoarthritis)
- Ultrasound (echo) – can visualize soft tissues and fluid accumulation
- Magnetic resonance imaging (MRI) – provides a detailed view of both bone and soft tissues and can reveal early signs of inflammation
- Computed tomography (CT) – useful for evaluating the structure of complex joints and bony abnormalities
Diagnostic criteria and differential diagnosis
Different arthritides have specific diagnostic criteria. The doctor must rule out or confirm various diagnoses, for example:
- Distinguish rheumatoid arthritis from osteoarthritis
- Identify gout based on the presence of uric acid crystals in the joint fluid
- Exclude infectious joint disease
- Evaluate whether joint symptoms are a manifestation of another disease, such as Lyme disease or psoriatic arthritis
The importance of early diagnosis
Early diagnosis is particularly important in inflammatory joint diseases because:
- Allows for the sooner initiation of appropriate treatment
- Reduces the risk of irreversible joint damage
- Better control of symptoms and slows disease progression
- Improves the long-term quality of life of patients
If you experience persistent or recurring joint pain, it is important not to delay and consult a specialist – a family doctor, who will refer you to a rheumatologist or orthopedist if necessary.
Treatment options: from medications to natural remedies
Treatment of arthritis is complex and individualized, tailored to the specific patient, taking into account the type of disease, symptoms, and general health. Modern medicine offers a variety of treatment strategies, from traditional medicines to natural methods.
Medication
Medication is the main tool in the fight against joint inflammation and its symptoms:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) – ibuprofen, diclofenac, naproxen, and others relieve pain and reduce inflammation. They can be taken in tablets or applied directly to the skin in the form of gels or ointments. Long-term use can cause gastrointestinal problems and increase the risk of cardiovascular disease.
- Corticosteroids – powerful anti-inflammatory drugs that can be prescribed in tablets or injected directly into the affected joint. They quickly reduce inflammation, but due to possible side effects, they are usually prescribed for short courses.
- Disease-modifying antirheumatic drugs (DMARDs) – methotrexate, sulfasalazine, leflunomide and others. These drugs slow the progression of the disease, especially in cases of rheumatoid arthritis, by suppressing the immune system. Their effect occurs after several weeks or months.
- Biologic drugs – a newer class of drugs designed to specifically target parts of the immune system involved in inflammation (e.g. TNF inhibitors). They are particularly effective in severe rheumatoid arthritis.
- Painkillers – paracetamol and opioid analgesics can be used to control pain when NSAIDs are insufficient or contraindicated.
Non-pharmacological measures
Medications are not the only way to manage joint inflammation. Physical therapy and other non-pharmacological measures play an important role:
- Physical therapy and physiotherapy – specific exercises designed to strengthen the muscles around the affected joints, improve flexibility and range of motion, and reduce pain.
- Weight management – weight loss can significantly reduce the load on the joints, especially the knees and hips, thereby reducing pain and slowing the progression of the disease.
- Heat and cold therapy – heat (hot compresses, heating packs) relaxes muscles and improves blood circulation, while cold (ice packs) reduces swelling and relieves acute pain.
- Orthopedic braces and assistive devices – can help reduce the load on the affected joints, correct incorrect posture, and facilitate daily activities.
Natural Supplements and Nutrients
Studies show that some natural supplements may be beneficial for joint health:
- Omega-3 fatty acids – have anti-inflammatory properties and may reduce joint pain and stiffness.
- Glucosamine and chondroitin – may help rebuild joint cartilage and slow its breakdown.
- Turmeric – its active compound curcumin has anti-inflammatory properties.
- Vitamin D – is important for bone health and may have a positive effect on the immune system.
- MSM (methylsulfonylmethane) – may help reduce inflammation and support joint health.
Explore our joint-strengthening supplements, which contain targeted nutrients like collagen, omega-3s, and more, trusted by those managing inflammation.
Surgical Options
When conservative treatments are not effective enough, surgical intervention may be considered:
- Joint replacement surgery – replacing a damaged joint with an artificial implant, most often performed on the knee and hip joints.
- Arthroscopy – a minimally invasive procedure that allows a surgeon to examine, diagnose, and treat joint problems.
- Joint arthrodesis – a fusion of a joint, where two bones are fused together to reduce pain but limit mobility.
- Synovectomy – removal of synovial tissue in a joint to reduce inflammation.
Complementary and alternative therapies
Many people seek additional ways to relieve joint pain:
- Acupuncture, a traditional Chinese medicine method that can help reduce pain.
- Massage, which can relax tense muscles and improve circulation.
- Mindfulness and stress management techniques, which can help you cope better with pain and reduce stress, which can exacerbate inflammation.
- Yoga and tai chi, which are gentle movements that help maintain flexibility and strengthen the muscles around your joints.
A personalized treatment plan
It’s important to understand that there is no one-size-fits-all treatment plan for everyone with arthritis. The treatment strategy must be tailored to each patient individually, taking into account:
- The type and severity of arthritis
- The joints affected
- The patient’s age and overall health
- Lifestyle and daily activities
- Previous response to treatment
The most effective treatment is often a combination of methods, from medications to lifestyle changes. It is always important to consult a healthcare professional before starting any new treatment regimen, especially if it involves taking supplements or alternative therapies.
How can you prevent arthritis and strengthen your joints?
While some risk factors, such as genetics or age, cannot be controlled, there are many ways to reduce your risk of arthritis and strengthen your joint health. Prevention and early intervention can help keep your joints healthy for the long term.
Regular physical activity
Exercise is one of the most important factors in maintaining healthy joints:

- Low-intensity aerobic exercise – swimming, walking and cycling – strengthens the muscles around the joints without putting too much strain on the joints.
- Strength training – it is important to strengthen the muscles around the joints, as they help absorb shock and reduce the load on the cartilage.
- Flexibility exercises – regular stretching exercises help maintain joint mobility and prevent stiffness.
- Aquatic sports – are especially beneficial for those who already have joint problems, as water reduces the effect of gravity on the joints.
- Yoga and Pilates – these exercises improve posture, strengthen deep muscles and increase overall body flexibility.
Weight management
Excess weight is one of the biggest risk factors for joint diseases:
- Every extra kilogram puts extra strain on weight-bearing joints, especially the knees, hips and back.
- Obesity also promotes systemic inflammation in the body, which can aggravate arthritic conditions.
- Even a small weight loss (5-10%) can significantly reduce joint pain and improve function.
Anti-inflammatory Diet
Certain foods can help control inflammation in the body:

- Omega-3 fatty acids – found in oily fish (salmon, mackerel), flaxseed, walnuts.
- Antioxidants – abundant in brightly colored fruits and vegetables, help fight free radicals that promote inflammation.
- Anti-inflammatory properties of spices – turmeric, ginger, cloves and cinnamon can help reduce inflammation.
- Polyphenols – found in green tea, red wine, dark berries, have anti-inflammatory properties.
It is also worth avoiding foods that can promote inflammation:
- Refined carbohydrates and sugars
- Trans fats and excessive saturated fat
- Processed foods and red meat (in large quantities)
- Alcohol (especially in the case of gout)
- Proper ergonomics and injury prevention
Joint injuries can increase the risk of arthritis in later life:
- Ergonomic workstations – proper chair height, computer screen position, wrist rest for the keyboard can reduce the load on the joints.
- Proper warm-up and cool-down procedures – before and after intense physical activity, reduce the risk of injury.
- Protective equipment – knee pads, wrist braces and proper footwear can protect joints from damage.
- Correct lifting technique – using your legs, not your back, to lift heavy objects.
- Overload prevention – regular breaks between repetitive movements and appropriate training intensity.
Stress management, sleep and rest
Stress and lack of sleep can worsen inflammatory processes:
- Regular rest – joints need time to recover after physical exertion.
- Sufficient sleep – tissue repair occurs during sleep and inflammation decreases.
- Stress reduction techniques – meditation, deep breathing and mindfulness practices can reduce levels of the stress hormone cortisol, which can promote inflammation.
- For additional tips on how to maintain strong joints, see our guide to maintaining healthy joints.
Regular health check-ups
Early detection of joint problems can prevent more serious damage:
- Visit your doctor regularly, especially if you have risk factors (family history, previous injuries).

- Don’t ignore persistent or recurring joint pain – it could be an early sign of inflammation.
- Monitor your vitamin D levels, especially during the winter months, as a deficiency has been linked to a higher risk of arthritis.
Joint health is a long-term commitment that requires attention in many areas of life. Fortunately, many of the factors that help maintain healthy joints are also beneficial for overall health – a balanced diet, regular physical activity and stress management are cornerstones of a healthy lifestyle.
FAQ: Frequently Asked Questions
What are the first signs of arthritis?
Early symptoms usually include joint pain, stiffness and sometimes swelling or redness, especially in the morning or after periods of inactivity.
What causes arthritis to worsen?
Flare-ups can be triggered by stress, increased physical activity, infections, changes in weather conditions or stopping medication/supplements.
Can arthritis be completely cured?
Acute arthritis can go away completely; Chronic forms can often be controlled but not completely cured—early diagnosis and treatment are essential.
What foods or nutrients help with joint health?
An anti-inflammatory diet rich in omega-3 fatty acids, antioxidants, and vitamins D and C (e.g., fatty fish, berries, leafy greens) supports joint health.
When should you see a doctor about joint pain?
If the pain lasts longer than a week, is severe, or is accompanied by swelling, redness, decreased mobility, or fever—see a specialist.