Antibiotics are some of the most commonly used drugs in the world to help fight bacterial infections. However, along with their beneficial effects, they can cause unpleasant side effects, especially for the intestinal microflora. Antibiotics do not divide bacteria into “good” and “bad” – they destroy all of them, including those that support a healthy digestive system. This is where probiotics come to the rescue – live bacteria and yeasts that, when used properly, can help restore a disrupted intestinal microbiome.
In this comprehensive guide, we will discuss how antibiotics affect the intestinal ecosystem, why it is worth taking probiotics after a course of antibiotics, and most importantly – how to do it correctly to get the maximum benefit. We will rely on the latest scientific knowledge and recommendations from doctors to help you make informed decisions about your health. We will find out which types of probiotics are the most effective, when to take them and how to choose the right products from the wide range of products on the market. You can learn more about probiotics and other microorganisms that are important for your digestion in our dictionary for your gut: probiotics, sporabiotics and prebiotics.
The effects of antibiotics on the gut microflora
Our intestines are home to trillions of microorganisms that form a complex ecosystem called the gut microflora or microbiota. These bacteria perform a variety of important functions, from absorbing nutrients to strengthening the immune system.
When we take antibiotics, this delicate balance is disrupted.
Antibiotics are broad-spectrum antibiotics—they are designed to kill the bad bacteria that cause infection, but they also kill many of the good bacteria in your gut. Think of it like a forest fire—it doesn’t discriminate between which trees it burns and which it leaves behind.

The result is a drastic reduction in the diversity and number of bacteria, which leads to a microbial imbalance called dysbiosis.
Studies show that after a course of antibiotics, the intestinal microflora can recover for several months or even longer. Some studies have even found that certain types of bacteria may not return without specific intervention. Such an imbalance can have a variety of negative consequences:
- antibiotic-induced diarrhea (occurs in 5-30% of patients)
- bloating and discomfort
- loss of appetite
- increased sensitivity to certain foods
- risk of opportunistic infections such as Clostridium difficile
- long-term effects on the immune system
Common symptoms after antibiotics
Many patients notice changes in their digestive system after a course of antibiotics. The most common of these are diarrhea, constipation, abdominal pain or discomfort, increased gas, and loss of appetite. These symptoms are usually temporary, but for some people they can last for weeks or even months, significantly reducing their quality of life.
Of particular concern is Clostridium difficile (C. diff) infection, which can develop when antibiotics kill off competing bacteria in the gut, allowing the pathogen to thrive. C. diff infection can cause severe diarrhea, fever, dehydration, and more serious complications, especially in older patients or those with weakened immune systems.
Why is it worth taking probiotics after antibiotics
Scientific studies increasingly clearly confirm the benefits of probiotics after antibiotic therapy. They act as “good bacteria” that help restore damaged intestinal ecology and reduce the side effects caused by antibiotics.
One of the main arguments in favor of probiotics after antibiotics is their ability to significantly reduce the risk of antibiotic-induced diarrhea. Studies show that taking certain probiotics can reduce the likelihood of this complication by as much as 50%. Probiotics not only reduce the risk of diarrhea, but can also help:
- restore the diversity of intestinal microflora faster
- strengthen the barrier function of the intestine
- support the activity of the immune system
- reduce the risk of opportunistic infections
- improve the absorption of nutrients
Lithuanian gastroenterologists are also increasingly recommending probiotics as an additional measure in combination with antibiotic therapy, especially for patients who have previously experienced digestive disorders after a course of antibiotics or have other risk factors.

Probiotics are especially beneficial after taking broad-spectrum antibiotics, which are the most damaging to the gut microbiome. They are also recommended for children, the elderly, and those with weakened immune systems or chronic digestive disorders.
Natural probiotics are found in fermented foods, while dietary supplements often offer concentrated and targeted benefits. You can find detailed information about the various options in our collection of natural gut support supplements.
How to Take Probiotics with Antibiotics – Timing, Forms, and Best Practices
To get the maximum benefit from probiotics while taking antibiotics, it is important to follow certain rules. While probiotics are safe for most people, the timing and method of their use can have a significant impact on their effectiveness.
Rules for Taking Probiotics After Antibiotics
1. When to Start Taking It? It is optimal to start taking probiotics on the same day you start your course of antibiotics. There is no need to wait until the course of antibiotics is over – this reduces the beneficial effect. Studies show that early probiotic use can reduce the extent of dysbiosis and speed up recovery.
2. Time gap between antibiotics and probiotics. It is very important to maintain a 2-4 hour gap between taking antibiotics and probiotics. For example, if you take antibiotics in the morning and evening, you can take probiotics at noon and before bed. This helps ensure that the antibiotics do not destroy the probiotic bacteria that you have just taken.
3. Duration of use. It is recommended to continue taking probiotics for at least 2 weeks after the end of the course of antibiotics. In cases of more severe dysbiosis or recurring problems, doctors may recommend a longer course of 4-8 weeks.
4. Forms of probiotics. There are various forms of probiotics on the market:
- capsules – convenient to take, often have protective technologies to ensure the survival of the bacteria
- powders – easy to dose, suitable for children and those who cannot swallow capsules
- liquid forms – quickly absorbed, but often require refrigeration
- fermented foods – natural source, but with a lower standardized dose
5. Dosage and product selection. Look for products that contain:
- multi-strain formulas (at least several species of bacteria)
- sufficient CFU (colony-forming units) – ideally 10-20 billion per day
- acid-resistant capsules to ensure the bacteria reach the intestines
- well-documented bacterial strains (e.g. Lactobacillus rhamnosus GG, Saccharomyces boulardii)
6. Precautions. Some people should be cautious with probiotics. Talk to your doctor before taking probiotics if you:
- have a severely weakened immune system
- suffer from serious intestinal conditions
- have recently had surgery
- are pregnant or breastfeeding
- are taking probiotics for young children
Probiotic foods or supplements
Natural sources of probiotics and supplements have their own advantages and disadvantages. Probiotics found in foods are generally better absorbed with food, but the amount of bacteria they contain is often smaller and less standardized.
The richest natural sources of probiotics are:
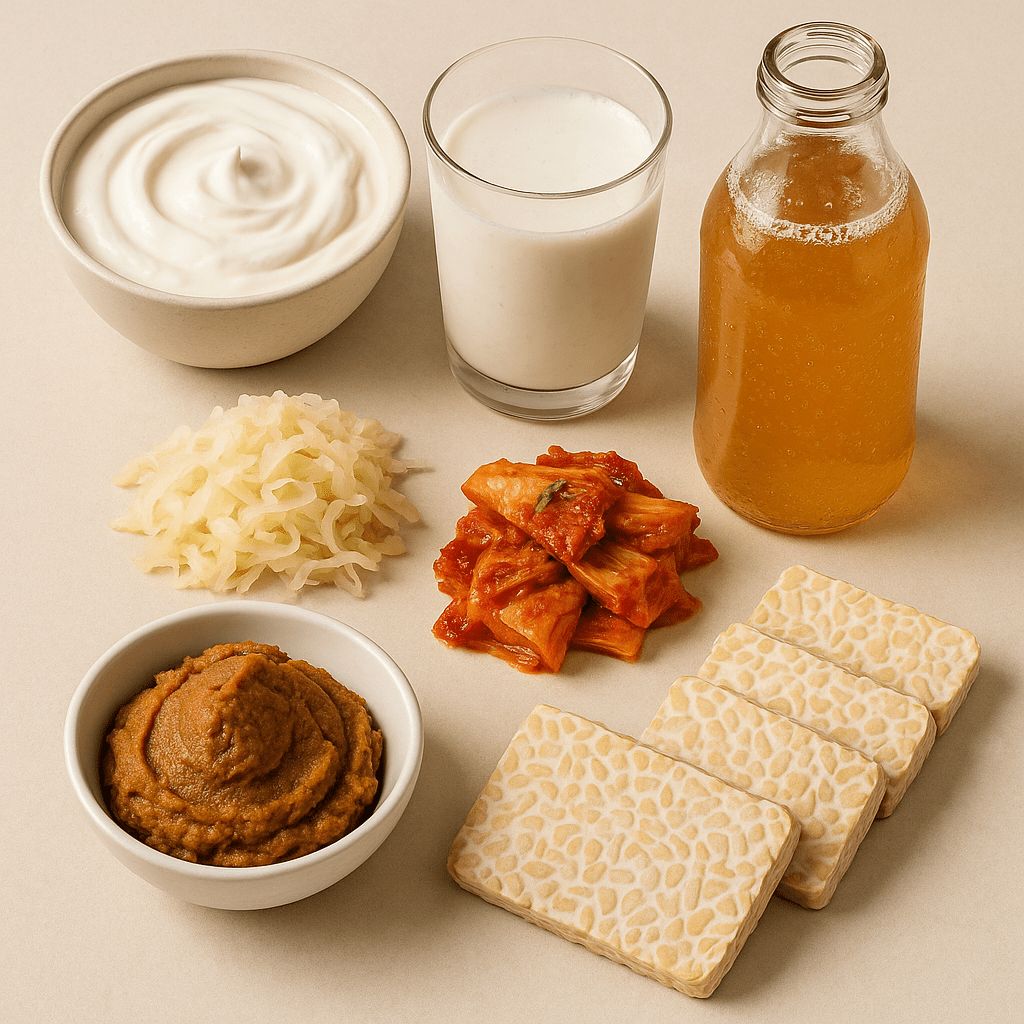
- fermented milk and yogurts with live cultures
- kefir – a particularly valuable source of multi-strain probiotics
- sauerkraut (unpasteurized)
- kimchi – a Korean fermented vegetable dish
- miso paste
- kombucha – a fermented tea drink
- tempeh – a fermented soy product
Probiotics work best in combination with prebiotics – fibers that feed good bacteria. If you are interested in how to strengthen immunity naturally, it is worth familiarizing yourself with our information on vitamins for immunity – these are natural food supplements that can be a great addition to probiotic therapy.
Choosing and purchasing probiotics: what to pay attention to
When choosing probiotics after a course of antibiotics, it is important to pay attention to several essential aspects that will ensure maximum effectiveness. The market offers many options, so being able to choose quality products is very important.
First of all, you should pay attention to the strains of bacteria. Studies show that different strains have different effects. The following strains are particularly useful after antibiotics:
- Lactobacillus rhamnosus GG – one of the best-studied strains, effective in reducing antibiotic-induced diarrhea
- Saccharomyces boulardii – a type of yeast, particularly effective against C. difficile infection
- Bifidobacterium lactis – helps restore the colonic microflora
- Lactobacillus acidophilus – improves overall intestinal function
Second, pay attention to the product’s formula. Multi-strain products (with several different strains of bacteria) tend to work better than single-strain probiotics. This is because different good bacteria colonize different parts of the gut and perform different functions.
Third, the concentration (CFU – colony-forming units) is very important. The recommended dose after antibiotics is at least 10-20 billion CFU per day. The packaging should clearly state the concentration of bacteria and a guarantee that it will last until the expiration date.
It is also important to pay attention to the following aspects:
- Shelf stability – does the product require refrigeration
- Preservative technologies – are there technologies that help the bacteria survive the acidity of the stomach
- Added ingredients – avoid products with high sugar content, artificial sweeteners or colorings
- Third-party certifications – independent quality assurance
- Expiration date – the bacteria are alive, so the product has a clear expiration date
Different age groups and needs may require different forms of probiotics. For example, drops or powders that can be mixed with food are suitable for babies and young children. Older people who have swallowing problems may also find it more convenient to take liquid or powder forms.
If you are considering starting probiotics after a course of antibiotics, it is worth comparing our carefully selected collection of probiotics tailored to your needs. Pharmacists often recommend assessing your specific health needs and possible interactions with other medications you are taking, so it is always worth consulting a specialist.
Conclusions
Probiotic supplementation after antibiotic therapy is becoming an increasingly important health care strategy to help reduce the side effects of antibiotics and restore a healthy gut microbiota more quickly. Current research supports the benefits of probiotics not only in reducing the risk of diarrhea, but also in supporting overall digestive health and immune response.
To get the most out of your probiotics, it is important to follow a proper regimen – start probiotics with antibiotics (2-4 hours apart), choose the right form and concentration, and continue taking them for at least two weeks after your antibiotic course. Keep in mind that different types of probiotics may work for different people, and in some cases, you should consult your doctor before using them.
Probiotics are not a panacea, but their scientifically based use can significantly contribute to faster recovery from antibiotic therapy and help prevent unpleasant complications. It is worth choosing a high-quality, research-based product and, if possible, combine dietary supplements with natural probiotic foods and a healthy diet.
By taking care of your gut health, you are investing in your overall well-being, stronger immunity, and better quality of life. However, remember that every body is unique, so the ideal solution is always an individual consultation with a healthcare professional.
Frequently Asked Questions (FAQs)
When should I start taking probiotics if I’m taking antibiotics?
Start taking probiotics the same day you start taking antibiotics, but leave 2-4 hours between doses.
How long should I continue taking probiotics after a course of antibiotics?
Many experts recommend continuing to take probiotics for at least 2 weeks after the end of your course of antibiotics, or longer if symptoms persist.
Are natural probiotic foods as effective as supplements?
Fermented foods are beneficial, but they may contain unstandardized amounts or specific strains; supplements ensure precise dosing.
Can probiotics prevent all side effects of antibiotics?
Probiotics significantly reduce the risk of antibiotic-associated diarrhea, but they may not protect against all side effects.
Are probiotics safe for everyone?
Most people tolerate probiotics well, but individuals with weakened immune systems or specific health conditions should first consult a healthcare professional.